مجلات علمية

People suffer from different skin diseases.
Discoid eczema is one of these diseases that hurts them. So, we should know about it and find a suitable cure.
What is discoid eczema?
It is a chronic skin disease that causes the skin to be itchy, cracked, and swallows making oval or circular patches on it.
It is also called nummular dermatitis and is defined by coin-shaped and sized plaques with small scales or yellowish crusts.
It isn't a contagious disease, so it can't be caught by touching the affected person.
Causes of discoid eczema
The main cause is unknown. But some cases are associated with the infection of staphylococcus aureus which may cause pus and weeping.
It may be associated with the following:
1-Dry skin
2-Contact dermatitis
3-Varicose veins
4-Wound infection or impetigo
5-A localized injuries like a thermal burn, insect bite, or scratch.
It can occur in association with atopic eczema, secondary schematization, and eczema craquelé.
Drug-induced discoid eczema may be due to medications causing dryness in the skin.
People affected by discoid eczema
It affects all age groups but according to the American Academy of Dermatology (AAD), it is slightly more affecting older adult males between the ages of 55 and 65 years and younger females starting from the teenage years or young adulthood.
It is associated with chronic alcoholism in men.
Clinical features of Discoid eczema
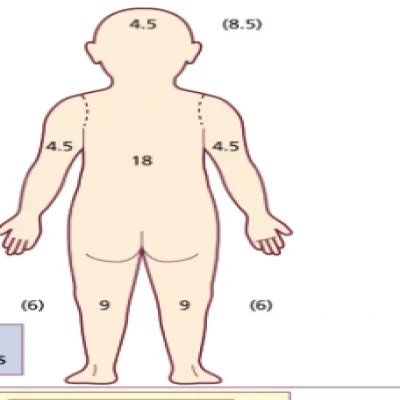
It usually affects the limbs, particularly the legs with a widespread rash.
It is often bilateral but its distribution can be asymmetrical especially when it is related to varicose veins.
The affected area is extremely itchy, especially at night, and it may burn or sting.
Continuous scratching and rubbing can lead to lichenification, in which the epidermis, or outer layer of skin, becomes overgrown.
This leads to thick skin, and exaggerated skin markings appear, making the skin look like leathery bark.
Discoid eczema has two clinical forms
1-Exudative acute discoid dermatitis
It is oozy papules, plaques, and blisters.
2-Dry discoid dermatitis
It is subacute or chronic erythematous, dry plaques.
Each plaque is 1-3 cm in diameter, well-circumscribed, and inflamed. Most of the patches are oval or round with dry and irritable skin between them.
Several small to large itchy plaques all over the body appear in generalized severe cases due to an autoeczematization reaction.
The patches may clear up without signs but in dark skin, marks may persist for a long time as pale postinflammatory hypopigmentation or dark brown postinflammatory hyperpigmentation.
Diagnosis of discoid eczema
It is characterized by:
1-Bacterial swaps may reveal Staphylococcus aureus infection or colonization.
2-Scrapings which are commonly taken for mycology, as discoid eczema looks similar to tinea corporis (ringworm infection).
3-Contact allergy to metals like nickel and chromate has been commonly reported. So, patch testing should be considered in chronic cases.
The differential diagnosis of discoid eczema
It may resemble the other annular skin eruptions like pityriasis rosea, tinea corporis, and plaque psoriasis.
But it must be differentiated from other infections because correct diagnosis will make appropriate treatment possible.
An example of the confusion
It is sometimes confused with a fungal infection called ringworm which can affect any type of skin but discoid dermatitis usually affects dry skin.
It is known that discoid eczema starts as very small, red spots that become a rash but ringworm is a circular patch that grows and becomes lighter in the middle, forming a ring. Both rashes can itch, but eczema causes a burning sensation.
The treatment of discoid eczema
Because it is associated with loss of skin barrier function, it is important to:
Protect the skin from any injury.
It often begins after minor skin injuries, so skin protection is required. If the hands are injured, use gloves and tools to ensure the skin is not irritated by detergents, friction, solvents, other chemicals, or excessive water.
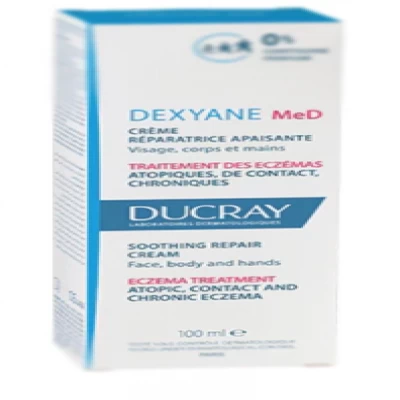
Using frequent emollient
Use types that include bath oils, soap substitutes, and moisturizing creams.
They can be applied to eczema frequently to relieve itching, dryness, and scaling.
Emollients should be used on the unaffected skin to reduce dryness.
It is necessary to try different products to find the suitable one.
Many people find one or more of the following is good like glycerine and cetomacrogol cream, white soft paraffin with liquid paraffin mixed, wool fat lotions, fatty cream, or urea cream.
Avoiding allergens
If patch testing identified contact allergies, the patient should avoid exposure to the allergens.
Using anti-inflammatory treatments which include:
1-Topical steroids
They are anti-inflammatory ointments or creams that are applied on the patches once or twice daily and used for 2-4 weeks.
They reduce symptoms and clear eczema.
2-Antibiotics
They are prescribed if it is sticky, crusted, or blistered.
It sometimes clears by using oral antibiotics but it recures if they are discontinued.
Examples of antibiotics used are erythromycin and flucloxacillin.
Other treatment used for severe discoid eczema
Antihistaminic pills reduce the itching of but they don't clear the rash.
Ultraviolet radiation therapy(UV)
It is used in case of generalized or widespread discoid eczema which can reduce itch and improve the rash.
It is phototherapy used several times weekly for 6–12 weeks.
It must be controlled to avoid the risk of premature skin aging or skin cancer.
Steroid injections
They are systemic steroids that are used for extensive cases.
They are used for a few weeks before continuing topical steroids and emollients on residual eczema.
Other oral treatments
It is like methotrexate, azathioprine, and cyclosporine.
They are used for Persistent and troublesome eczema.
They require careful monitoring by a specialist dermatologist. They may be more suitable than long-term systemic steroids.
Prevention of discoid eczema
Some tips help in reducing the recurrence of the infection.
1-Trying an air humidifier in the home.
2- Hydrating the skin by moisturizing and adding oils to the bath.
3- Avoiding hot baths and showers.
4- Avoid using the soap
5- Wearing loose clothes that don't irritate the skin, and choose natural, rather than man-made fabrics.
6- Dry the skin gently with a soft towel, after bathing.
7- Using a laundry detergent that isn't irritating to the skin.